Welcome to another edition of Nutrition Stories, a series exploring hot topics in nutrition and dietetics. Our guest is Courtney Piltaver, a graduate of the UF Didactic Program in Dietetics (DPD) in the Food Science and Human Nutrition (FSHN) Department at The University of Florida. In this article, Courtney shares her experiences with a postural orthostatic tachycardia syndrome (POTS) and offers research-based nutrition tips for those with POTS to discuss with their healthcare teams.
Welcome to another edition of Nutrition Stories, a series exploring hot topics in nutrition and dietetics. Our guest is Courtney Piltaver, a graduate of the UF Didactic Program in Dietetics (DPD) in the Food Science and Human Nutrition (FSHN) Department at The University of Florida. In this article, Courtney shares her experiences with a postural orthostatic tachycardia syndrome (POTS) and offers research-based nutrition tips for those with POTS to discuss with their healthcare teams.
Courtney:
Imagine starting each day not knowing if standing up might cause your heart to race, your head to spin, and your energy to drain. This has been my reality since being diagnosed with postural orthostatic tachycardia syndrome (POTS). POTS is a condition that turned my life into a daily puzzle of trying to manage my symptoms. However, it has also been a journey of self-discovery, especially in understanding the vital role nutrition plays.
The Onset of POTS Symptoms
 I can’t say I remember an exact moment that defines when my POTS symptoms started. What I do recall is noticing that sometimes when I stood up, I became dizzy and lightheaded, my vision went black, and I would almost pass out. I also experienced extreme fatigue, horrible headaches, and issues with temperature regulation.
I can’t say I remember an exact moment that defines when my POTS symptoms started. What I do recall is noticing that sometimes when I stood up, I became dizzy and lightheaded, my vision went black, and I would almost pass out. I also experienced extreme fatigue, horrible headaches, and issues with temperature regulation.
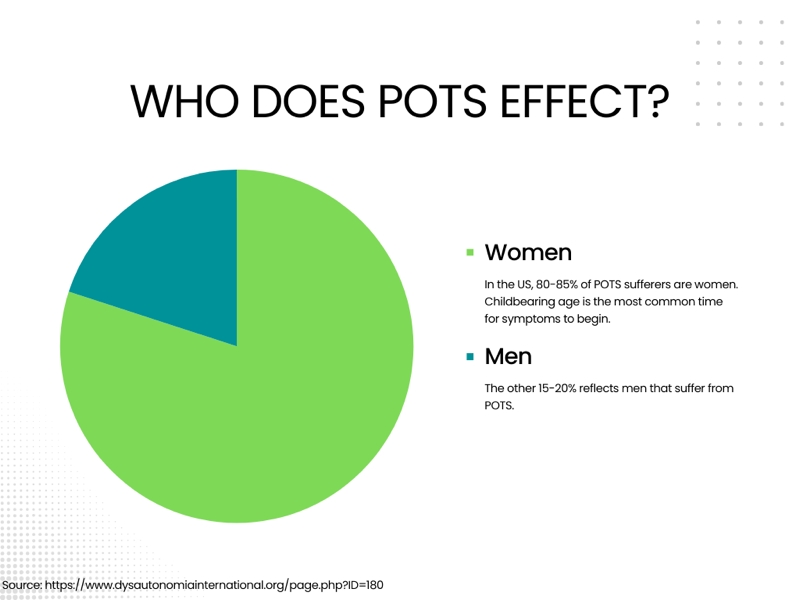
Over time, these symptoms that occurred upon standing only became more frequent, and sometimes I actually passed out. This worrying change led me to see a functional medicine doctor, who diagnosed me with POTS. I met with a cardiologist to confirm this diagnosis through a tilt table test, which measures heart rate and blood pressure responses to change in posture. I learned that it affects 1 to 3 million people in the U.S., predominately young to middle-aged women.1 We don’t know why this condition mostly affects women, but research suggests it may be due to the vasodilation effects of female sex hormones, with testosterone having vasoconstrictive effects.1
POTS is a form of dysautonomia that affects the autonomic nervous system, causing an excessive increase in heart rate upon standing.2 Symptoms range from dizziness and fainting to fatigue and rapid heartbeat, each presenting unique challenges to daily life.2
The Role of Nutrition and Physical Activity in POTS Management
 Researchers have emphasized the importance of hydration and increased salt intake, alongside a balanced diet, to manage symptoms.3 With this newfound knowledge, I embarked on a personal journey to regain my balance–literally and figuratively. I experimented with my diet, incorporating more fluids and salt under medical guidance, and adjusted my meal sizes and frequency. These new methods proved to be gamechangers. Each small tweak in my diet brought me closer to feeling like myself again, underscoring the significant role nutrition plays in POTS.
Researchers have emphasized the importance of hydration and increased salt intake, alongside a balanced diet, to manage symptoms.3 With this newfound knowledge, I embarked on a personal journey to regain my balance–literally and figuratively. I experimented with my diet, incorporating more fluids and salt under medical guidance, and adjusted my meal sizes and frequency. These new methods proved to be gamechangers. Each small tweak in my diet brought me closer to feeling like myself again, underscoring the significant role nutrition plays in POTS.
However, nutrition was just one piece of the puzzle. In addition to dietary changes, incorporating gentle physical activity tailored to individual symptoms was important.2 Exercise like Pilates can help improve cardiovascular fitness without triggering symptoms. On days when symptoms were more challenging, medications like propranolol helped regulate blood volume and heart rate, providing effective symptom relief.2
 Hydration and Dietary Adjustments
Hydration and Dietary Adjustments
Hydration emerged as another factor I found helpful in my symptom improvement. My doctor recommended increasing my fluid intake to at least two to three liters per day and adding more salt to my diet to help expand my blood volume, a strategy supported by research.3 My doctor also suggested a hydration packet, which significantly helped sustain my energy throughout the day. Oral rehydration therapy is a general practice for treating POTS, as it provides more electrolytes and helps sustain hydration in POTS patients.4
Initially, adding more salt felt counterintuitive, especially as a dietetics major. Isn’t too much salt supposed to be bad for you? However, in cases of POTS, where blood can often pool in the legs due to standing, these adjustments in salt intake and hydration can be very helpful.3
Smaller, more frequent meals can also help manage POTS symptoms by preventing significant shifts in blood volume that occurs after eating large meals, which can worsen symptoms.2 Starchy carbohydrates are known for providing energy to the body, but for POTS, symptoms may worsen after eating a high carb meal.5 Blood moves to the gut to aid in digestion and can lead to a drop in blood pressure.5
 Managing POTS Symptoms Through Nutrition
Managing POTS Symptoms Through Nutrition
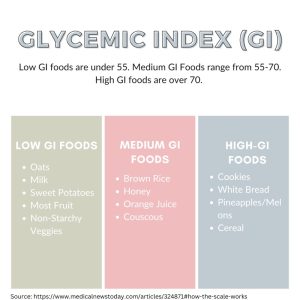
Replacing high carb food with high protein, healthy fats, and fiber can be beneficial in managing symptoms.6Foods high in sugar can cause spikes in blood sugar and insulin levels, leading to energy crashes and potentially worse symptoms, like fainting, fast heartbeat, sweating, and shakiness.2,6 Overall, focusing on complex carbs with a low glycemic index can help sustain energy and stabilize blood sugar.2 See the table below for more information regarding the glycemic index of foods.
Alcohol and caffeine can exacerbate symptoms for many individuals. Caffeine can be dehydrating, and while it can provide a temporary boost in blood pressure, it can also lead to heart palpitations and worsen tachycardia.3 Alcohol is a known diuretic, which can lead to dehydration and a decrease in blood volume, worsening symptoms.3 Each person experiences different symptoms with POTS. It is important to discuss options with a healthcare provider to find the best and most manageable way to address POTS.
 Continuing My Journey With POTS
Continuing My Journey With POTS
My journey with POTS is ongoing and is a path filled with many challenges and newfound knowledge. Along the way, I’ve learned the importance of advocating for myself, staying informed, and being open to adjusting strategies as needed. To those dealing with POTS, know that you are not alone. This journey is unique, but many of us understand what you’re going through.
Living with POTS requires you to manage symptoms, understand your body, and make daily choices that support your health. Through my journey, I’ve learned there’s no one-size-fits-all approach, and that living with POTS requires a combination of medical guidance, nutrition adjustments, and community support. I encourage those affected with POTS to explore these strategies, consult a healthcare professional, and find support within your community. Finally, consider sharing this article with loved ones to spread an understanding of POTS and to further help those that struggle with it.
Additional Resources
Strategies for managing POTS and support for sufferers
Learn more about dysautonomia
Testing and Diagnosing POTS
References
- Dysautonomia international: Lifestyle adaptations for POTS. Dysautonomiainternational.org. Accessed March 1, 2024. http://www.dysautonomiainternational.org/page.php?ID=44
- Fedorowski A. Postural orthostatic tachycardia syndrome: clinical presentation, aetiology and management. J Intern Med. 2019;285(4):352-366. doi:10.1111/joim.12852
- Di Baise Tisha N. Lunsford Lucinda A. Harris JK. The POTS (postural tachycardia syndrome) epidemic: Hydration and nutrition issues. Virginia.edu. Accessed March 1, 2024. https://med.virginia.edu/ginutrition/wp-content/uploads/sites/199/2019/06/POTS-June-2019.pdf
- Snapper H, Cheshire WP. Oral and intravenous hydration in the treatment of orthostatic hypotension and postural tachycardia syndrome. Auton Neurosci. 2022;238(102951):102951. doi:10.1016/j.autneu.2022.102951
- PoTS UK. Published September 13, 2021. Accessed March 26, 2024. https://www.potsuk.org
- Nutrition strategies for managing POTS. Standinguptopots.org. Accessed March 26, 2024. https://www.standinguptopots.org/nutritionstrategiesPOTS
Header photo credit: Henry Be on Unsplash.
Looking for more posts sharing stories about nutrition hot topics? Check out the rest of the UF/FSHN Nutrition Stories Series!
 3
3