We’re thrilled to bring you another edition of Nutrition Stories, our series exploring hot topics in nutrition and dietetics. Today’s guest is Emily Cohen, a graduate of the UF Didactic Program in Dietetics (DPD) and current master’s degree student in the Masters of Science – Dietetic Internship program in the Food Science and Human Nutrition (FSHN) Department at the University of Florida. In this article, Emily describes how folate deficiency in pregnant people with celiac disease can increase the risk of neural tube defects and other health issues in their children. Through screening and supplementation, this risk can be significantly reduced. Read on to learn how to detect and treat a folate deficiency.
We’re thrilled to bring you another edition of Nutrition Stories, our series exploring hot topics in nutrition and dietetics. Today’s guest is Emily Cohen, a graduate of the UF Didactic Program in Dietetics (DPD) and current master’s degree student in the Masters of Science – Dietetic Internship program in the Food Science and Human Nutrition (FSHN) Department at the University of Florida. In this article, Emily describes how folate deficiency in pregnant people with celiac disease can increase the risk of neural tube defects and other health issues in their children. Through screening and supplementation, this risk can be significantly reduced. Read on to learn how to detect and treat a folate deficiency.
Emily:
Research has shown that approximately 20-30% of adults newly diagnosed with celiac disease have a folate deficiency.1 For women of reproductive age, this deficiency can not only have implications on their own clinical outcomes, but also their future babies’ as folate deficiency in the first trimester of pregnancy has been linked to the development of birth defects.2
What is Celiac Disease?
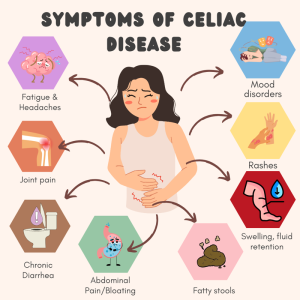
 Celiac disease is categorized as an autoimmune disorder that occurs due to variants in HLA-DQ2 and HLA-DQ8 genes. As a result, the immune system attacks the villi of the small intestine, causing them to atrophy.1 Since these villi play a crucial role in absorption of nutrients, this atrophy results in numerous deficiencies in essential vitamins and minerals such as iron, B12, calcium, vitamin D, and folate as well as malnutrition in the affected population.1 1 in 133 Americans are affected by this disease, playing a dramatic role in their overall nutritional and health status.
Celiac disease is categorized as an autoimmune disorder that occurs due to variants in HLA-DQ2 and HLA-DQ8 genes. As a result, the immune system attacks the villi of the small intestine, causing them to atrophy.1 Since these villi play a crucial role in absorption of nutrients, this atrophy results in numerous deficiencies in essential vitamins and minerals such as iron, B12, calcium, vitamin D, and folate as well as malnutrition in the affected population.1 1 in 133 Americans are affected by this disease, playing a dramatic role in their overall nutritional and health status.
While many people believe that the onset of celiac disease only occurs at a young age, the average age of diagnosis is 32 years old, close to the age many women become pregnant.1 Additionally, since the symptoms of celiac disease manifest in similar ways to other GI disorders with varying degrees of severity, the disease has a tendency to be undiagnosed or misdiagnosed for quite some time.1 In fact, there is an average delay of six to ten years before correct diagnosis.1
As a result, upon diagnosis, many patients have very minimal absorptive capacity due to long-term gluten ingestion, causing the degradation of the microvilli in the small intestine. This inability to efficiently absorb critical nutrients only exacerbates their malnutrition status.
 How is Celiac Disease Diagnosed?
How is Celiac Disease Diagnosed?
Diagnosis of celiac disease involves first screening for elevated levels of tissue transglutaminase IgA antibody (tTG-IgA).3 However, since this screening is only 93% sensitive to the disorder, the test is only a screening tool and not diagnostic of celiac disease. If the screening is positive, an endoscopic small intestine biopsy is required to confirm the diagnosis.3
If the test produces a negative result, more comprehensive screening such as genetic testing for the HLA-DQ2 and HLA-DQ8 gene variants or a gluten challenge is required before an intestinal biopsy can be performed. A gluten challenge comes secondary to the initial screening as this can exacerbate symptoms and is poorly tolerated among patients.4 If the patient is positive for the antibodies after the gluten challenge, a biopsy can then be performed to confirm the diagnosis.3
What is Folate and Why is it Important in Pregnancy?
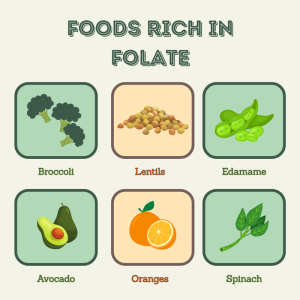
Folate is a water-soluble vitamin found in green leafy vegetables as well as certain legumes.1 This vitamin is essential for not only DNA synthesis and methylation, but also for the health of a newborn fetus. Because folate is required for DNA synthesis of red blood cells (RBCs), a folate deficiency can lead to megaloblastic anemia, a form of anemia where the RBC fails to mature, rendering them unable to divide and bind hemoglobin.1 Megaloblastic anemia manifests in tiredness, easy bruising, shortness of breath, and weakness as less oxygen can circulate through the body.1 While these symptoms are present in fully grown adults, the important role folate plays in DNA synthesis can also have an irreversible effect on a unborn fetus before pregnancy is confirmed.
 Folate Deficiency & Neural Tube Defects (NTDs):
Folate Deficiency & Neural Tube Defects (NTDs):
On the 28th day of pregnancy, the embryo’s neural tube closes, leading to the development of a spinal cord as well as the brain.2 However, inadequate folate status in the mother may cause failure of the neural tube to close, leading to irreversible birth defects such as spina bifida and anencephaly.2 Spina bifida is a condition in which the spinal cord and nerves are exposed, leading to paralysis as well as increased risk of infection.2 Anencephaly is a condition in which the brain, skull, and scalp is missing at birth, leading to brain death.2
Unfortunately, the average woman does not realize she is pregnant until she is six to eight weeks into pregnancy, after the neural tube closes at 28 days of pregnancy. Therefore, adequate folate status prior to pregnancy is essential to prevent these life-altering conditions and ensure a healthy fetus.2
How Do You Diagnose Folate Deficiency?
A folate deficiency as well as subsequent megaloblastic anemia can be diagnosed through blood draw markers.
Red Blood Cell Folate:
Due to the sensitivity of serum folate levels to short-term increase in folate intake, RBC folate has been introduced as the best indicator of long-term folate status.7 If this lab value is <150 ng/dL, it is indicative of a deficiency.7
Homocysteine:
Due to the buildup of homocysteine from a folate deficiency, serum homocysteine levels can be used to help determine folate deficiency.7 However, due to another vitamin’s (B12) role in homocysteine’s conversion to methionine, this marker is non-specific and may indicate a B12 deficiency. This screening is still common as an indicator of megaloblastic anemia, which can result from a vitamin B12 deficiency. Therefore, further tests are required to confirm diagnosis of celiac disease.7
Celiac Disease & Folate Deficiency: What are the Implications?
Folate from food is primarily absorbed in the small intestine. Therefore, villi atrophy resulting from celiac disease puts patients at risk for malabsorption and, consequently, a folate deficiency. A gluten-free diet will reduce villi atrophy. Yet due to mis-labeling of products, trace amounts of gluten sometimes remain in “gluten-free” foods.8 Additionally, due to cross contamination in “gluten-free” products, lack of education regarding the logistics of a gluten-free diet, the high cost of gluten-free foods, and other challenges to following a gluten-free diet, only 30-50% of those with celiac disease are able to fully adhere to the diet.9
Folate deficiency can lead to poor clinical outcomes in the prevention of cardiovascular disease, anemia, as well as many other neurological disorders.
For pregnant women, meeting increased energy needs can make following a gluten-free diet especially challenging, as many gluten-containing foods are key sources of energy.8As a result, adherence to a gluten-free diet in pregnancy becomes more difficult. Given the low rates of adherence to a strict gluten-free diet, folate deficiency remains a concern in the population after diagnosis and treatment. Celiac disease has also been linked to worse maternal and fetal outcomes during pregnancy.2
The Light at the End of the Tunnel: A Simple Solution
 Although the consequences of folate deficiency in pregnancy for those with celiac disease are severe, correcting the deficiency is relatively simple. First, if a patient experiences the common symptoms of a folate deficiency, they can ask their doctor to be screened for a folate deficiency. Moreover, for all woman of childbearing age, screening is recommended even if the patient is not currently trying to conceive.1
Although the consequences of folate deficiency in pregnancy for those with celiac disease are severe, correcting the deficiency is relatively simple. First, if a patient experiences the common symptoms of a folate deficiency, they can ask their doctor to be screened for a folate deficiency. Moreover, for all woman of childbearing age, screening is recommended even if the patient is not currently trying to conceive.1
If screening reveals a deficiency, oral supplementation of at least 400 mcg of folic acid per day resolves the deficit.1 At high pharmacological doses, folic acid is absorbed passively, meaning the villi of the small intestine are not needed for absorption.1 Therefore, regardless of intestinal absorptive capacity, folate status is improved.
A Screening That Saves Multiple Lives
Folate deficiency can lead to poor clinical outcomes in the prevention of cardiovascular disease, anemia, as well as many other neurological disorders. For those at reproductive age, awareness of this deficiency is especially important considering the development of a neural tube defect occurs before many women know they are pregnant.
In populations at special risk for this disease due to malabsorption, such as celiac disease, it is even more essential to be screened for the deficiency. Let’s help ensure the health of you and your future baby by getting screened. If a folate deficiency is found, talk with your doctor about supplementation of at least 400 mcg of folic acid/methylfolate to help protect the health of your future child.
References
- Martín-Masot R, Nestares MT, Diaz-Castro J, et al. Multifactorial Etiology of Anemia in Celiac Disease and Effect of Gluten-Free Diet: A Comprehensive Review. Nutrients. 2019;11(11):2557. doi:10.3390/nu11112557
- Lev L, Petersen K, Roberts JL, Kupferer K, Werder S. Exploring the Impact of Folic Acid Supplementation and Vitamin B12 Deficiency on Maternal and Fetal Outcomes in Pregnant Women with Celiac Disease. Nutrients. 2024;16(18):3194. doi:10.3390/nu16183194
- Celiac Disease Screening. Celiac Disease Foundation. Accessed March 13, 2025. https://celiac.org/about-celiac-disease/screening-and-diagnosis/screening/
- Fatigue Symptoms – Social Media. Canva. Accessed April 17, 2025. https://www.canva.com/design/DAGk7cBuF2Y/_j4Sr98684T5fHV25DS5jg/edit
- Foods Rich In Folate – Social Media. Canva. Accessed April 17, 2025. https://www.canva.com/design/DAGk7X3YnFo/0fwepqscq06Wrc34ers55A/edit
- Spina bifida. Dayton Children’s Hospital. Accessed November 13, 2025. https://fetaltonewborn.org/myelomeningocele-spina-bifida/spina_bifida-web-cdc/
- Snow CF. Laboratory Diagnosis of Vitamin B12 and Folate Deficiency: A Guide for the Primary Care Physician. Arch Intern Med. 1999;159(12):1289. doi:10.1001/archinte.159.12.1289
- Wieser H, Ruiz-Carnicer Á, Segura V, Comino I, Sousa C. Challenges of Monitoring the Gluten-Free Diet Adherence in the Management and Follow-Up of Patients with Celiac Disease. Nutrients. 2021;13(7):2274. doi:10.3390/nu13072274
- Folic Acid Supplement. Canva. Accessed November 13, 2025. https://www.canva.com/design/DAG4mnbLTJY/z0pHIFbXPxXkFZggQf9cYQ/edit
Looking for more posts sharing stories about nutrition hot topics? Check out the rest of the UF/FSHN Nutrition Stories Series!
 1
1